| Travelling on a train to Scotland, all for the first time: Clinical researcher says: "Look the cows in Scotland are black!". Physicist replies: "No. Some of the cows in Scotland are black" Mathematician says: "No, actually in Scotland there is at least one cow black on one side" |
I’ve written about folic acid, homocysteine and various clinical trials of nutrients in the past. I just want to revisit it briefly because I think there are some seriously wrong messages emerging from the conclusions. For an excellent comment on evidence based recommendations see Colby Vorland.
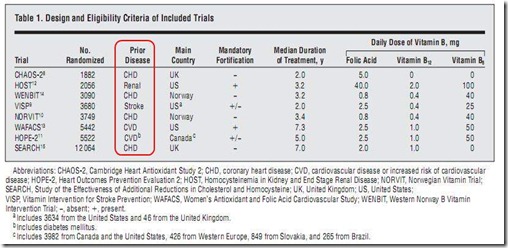
Homocysteine (Hcy) is associated with CVD, may or may not be causal but the evidence is good (Wald et al, BMJ, 2002). Folic acid (Vitamin B9) in reasonable amounts will lower homocysteine but clinical trials have been carried out, mostly showing not much benefit as far a CVD is concerned. A recent meta-analysis of 8 trials (total 37,485 individuals) seems to confirm this: “Dietary supplementation with folic acid to lower homocysteine levels had no significant effects within 5 years on cardiovascular events”.
BUT… all the studies were in ill people (mean age 65yrs), 7/8 with heart disease or stroke and 1 study on patients with kidney disease:
So a fair conclusion is that people who have already had a heart attack, stroke or some other sort of vascular disease may not benefit from homocysteine lowering – e.g. there was no reduction in second heart attacks, at least over the short term (mean 5 yrs).
Pity, but not so unexpected, after all vitamins are not medicines to be used when one becomes ill at 65 years old – vitamins are for life.
There are also several possibilities why Hcy lowering had apparently no effect on the patients, and also Wald et al point out that aspirin use may mask the effect of homocysteine lowering – it was interesting to see that they felt the need to underline what should be obvious:
“The fact that most of the trials included patients with pre-existing cardiovascular disease leaves open the possibility that folic acid has a useful role in the primary prevention of ischaemic heart disease, where aspirin is generally not used, but not in secondary prevention, where it is routine.”
So what do Clarke et al conclude? It’s starts off OK:
“The present meta-analysis has demonstrated that lowering homocysteine levels by an average of 25% (about 3 µmol/L) for an average of 5 years has no significant effect on the incidence of major vascular events during the scheduled treatment period.”
(They just missed out the aged ill patients bit)
They go on to discuss how observational and epidemiological studies associate homocysteine with cardiovascular disease and stroke (but do not point out that these studies were in the general population, not a diseased subset) and finally:
“One-third of adults in the United States and one-quarter of those in the United Kingdom report taking daily multivitamin supplements containing folic acid. The present meta-analysis, however, found no evidence that routine use of folic acid for 5 years has any material effect on cardiovascular or non cardiovascular events in the North American and European populations studied.”
These are two sentences from different contexts entirely – the results of the meta-analysis apply only to the study group and have NO bearing on the folic acid and homocysteine as far as primary prevention is concerned. The reviewers really should not have let that pass.
There is also a commentary on this article in the same issue which goes even further in the wrong direction. It begins discussing the role of vitamins in health and prevention then discusses the impact of the meta-analysis:
- Clarke and colleagues definitively answers most of the questions about the efficacy of B-vitamin therapy.
- There were no trends toward benefit in any of the primary outcomes overall or in the prespecified subgroups
- This is a cautionary tale for all who are searching for therapies to prevent disease in the general population.
But as the commentary says there is a “strong scientific rationale” for Hcy lowering and “consistent observational data from high quality cohort studies with more than 10 years of prospective follow-up confirmed the outcomes suggested by hypotheses arising from laboratory and animal data.”
This all remains true and has not been touched by any of the clinical trials but the author goes on:
“However, randomized trials of vitamin therapy with folate, vitamin B6, vitamin B12…demonstrated that none of these therapies are effective for preventing cardiovascular disease…in the general population.”
This is simply not true, the trials did not study the general population and have NO relevance at all for primary prevention. There’s more:
“As trusted counselors with an ethical mandate to first do no harm, we physicians should keep this history in mind as we advise our patients about the risks and benefits of dietary supplements… Vitamins taken in excess of the dose required to prevent deficiency states have not improved not improved our patients’ health and may harm them. We should recommend therapies to prevent disease in healthy patients only when randomized trials unequivocally demonstrate that net benefits outweigh net harms, and we should continue to emphasize the importance of a nutritious diet, regular physical activity, and no smoking as the best ways to optimize health.”
Couple of things: a) to not recommend is also a recommendation and b) how does the author know about the benefits of physical activity & nutritious diet and possible harms of smoking? All the evidence is from epidemiology and observation – they have not been confirmed by randomized trials!
Maybe the cows in Scotland are black.

Comments
Post a Comment